Participate in Making Austin a More Equitable City
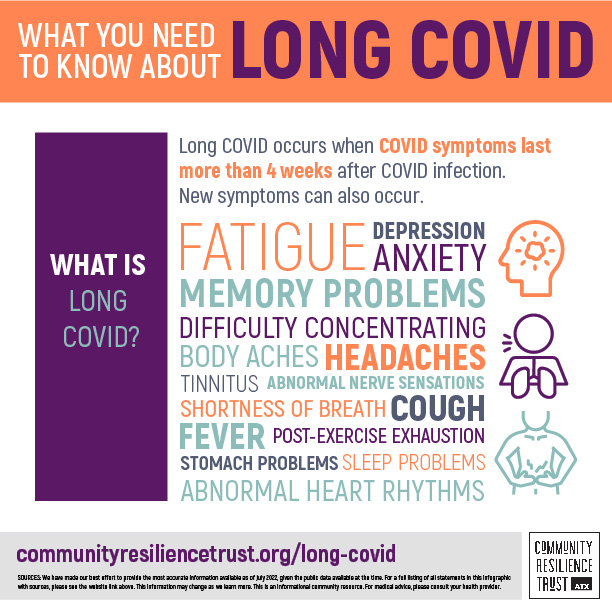
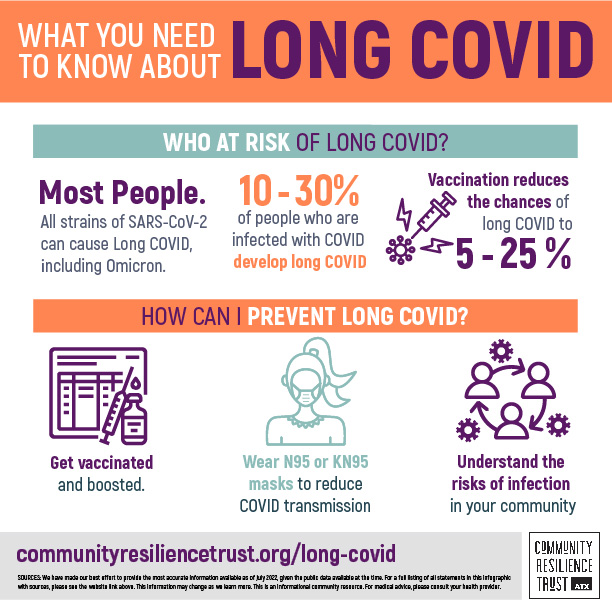
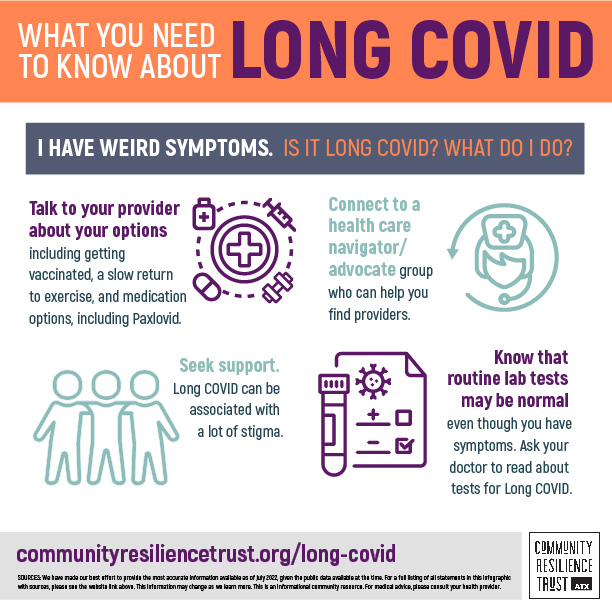
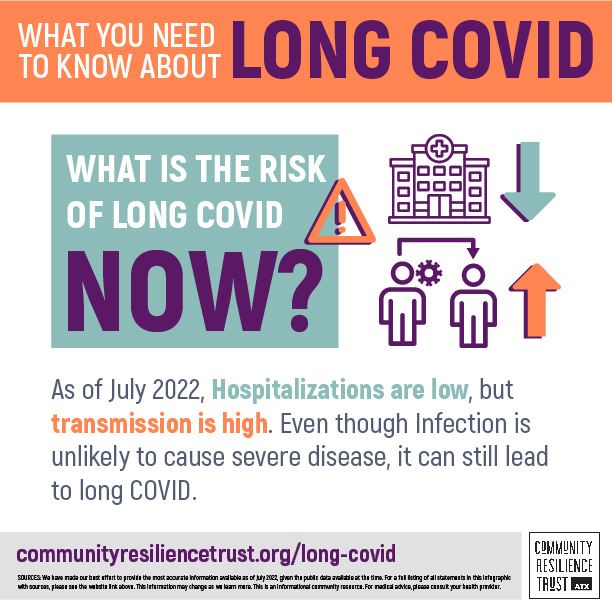
We are inviting you to participate our research to support the question “What is the impact of long COVID on POC in the Austin/Travis County area?” This is a preliminary study for community engagement and education, including providers.